Enhancing communications between primary care and secondary care mental health with an Advice and Guidance service
Published: 5 July 2021
Lancashire & South Cumbria NHS Foundation Trust (LSCFT) employs approximately 7,000 members of staff and has a turnover of more than £300m. The Trust has 517 inpatient beds spread across 40 wards, 16 of which are children’s mental health beds.
LSCFT also offers community-based services, including mental health, delivering more than 4,500 outpatient clinic appointments a week and in excess of 5,500 community clinic appointments a week.
Situation
In 2019, the Community Mental Health Team’s (CMHT) referral rate at LSCFT was shown to be 42% higher than the national average, according to national reporting data (NHS Digital, 2019). Anecdotally, some patients were having to wait up to 9 months to see a consultant psychiatrist due to these pressures.
Aspiration
The aspiration was to ensure that people with more complex mental health needs in primary care are able to access timely and responsive treatment.
This would mean facilitating appropriate care through specialist advice to the GP, to reduce the need for the patient to retell their story to multiple professionals in the course of a formal referral to secondary care. This would also reduce some of the pressures in specialist mental health services by reducing waiting times for those patients who do require active support delivered in secondary care.
Solution and impact
Two LSCFT community mental health teams (the single point of access team and the memory assessment service) implemented an electronic messaging system to allow GPs to contact consultant psychiatrists directly for clinical advice.
The Advice and Guidance service has created a streamlined care pathway for patients to receive necessary healthcare in a speedier manner by opening up a formalised channel of communication between secondary and primary care. This aligns with the ambitions of the NHS Long Term Plan and 5 Year Forward View.
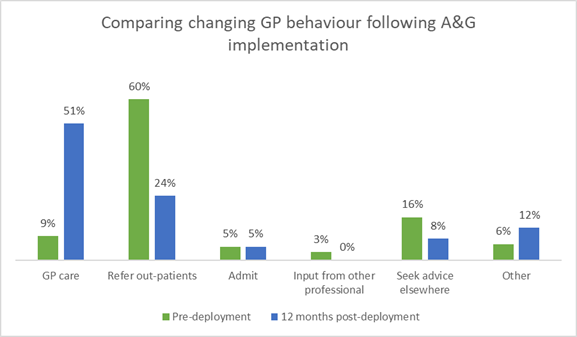
The service has led to a change at LSCFT in how GPs manage cases:
- GP self-management of cases has increased from 9% pre-implementation, to 51% post-implementation
- Before the system, the queries raised via the A&G platform would have resulted in a referral to secondary care in 60% of cases. This reduced to 24% following the availability of rapid specialist advice
- 100% of GPs reported on the ease of use of the system
- 92% reported that the advice provided by the psychiatrists was ‘really useful’ or ‘useful’
In terms of qualitative data, and through individual interviews and a focus group, the following have been noted from GPs and psychiatrist feedback:
- opportunities to harness rapid specialist advice for use in primary care
- ability to provide assurance to patients that care is being managed with documented specialist advice
- reduction in unnecessary appointments for patients
- quicker care for patients
- provision of specialist care for those who would otherwise not be able to access it
- for GPs - improved access to psychiatrists guidance for GPs
- for psychiatrists - better sense of collaboration with GPs
Functionality
The LSCFT Advice and Guidance system is a web-based system, which enables clinicians in different settings to communicate with each other. A local acute Trust (University Hospitals of Morecambe Bay Foundation Trust - UHMB) developed the system to enable primary care clinicians to seek clinical advice from secondary care clinicians. This has been adopted by LSCFT with the support and guidance from the technical team at UHMB.
Capabilities
- The LSCFT Advice and Guidance system is embedded in the electronic record (EPR) system for all GP practices (EMIS), so GPs who want to raise a query can click through from their EPR. A dialogue box opens in which they can then write the clinical query and they can also attach a file to the message if required. If GPs would prefer to be contacted by phone they can use the date/time picker to indicate their availability, which is then also sent alongside the query. Specific patient details are automatically pre-populated
- The clinical query can be directed to a central email inbox and the identified recipients (in this case the consultant psychiatrists in the team) take ‘ownership’ of an individual query and respond to the query as appropriate
- There is no limit to the number of messages that can be sent by either party in the conversation. However, the query can only be marked as ‘closed’ by the GP
- On closure, the system displays a mandatory questionnaire for GPs with 4 questions and an optional free text box for comments. This enables GPs to provide information for the impact on the patient journey (pre and post-advice and guidance), feedback on the ease of use of the system, and suggestions on how the system could be improved (free text)
- Once closed, the conversation automatically feeds into the EMIS clinical record
- Back-end reporting is built into the system capturing data utilising Qlikview and SQL server reporting services
Scope
The LSCFT Advice and Guidance system enables GPs to use their EPR system to directly contact consultant psychiatrists working in the single point of access team and the memory assessment service for clinical advice. This allows patients to rapidly access a collaborative model of specialist support involving the GP in primary care and the consultant psychiatrist in secondary care.
The system is for routine clinical advice and not for emergency queries.
Key learning points
Service engagement
Ensure that the all staff impacted by the system deployment are included in all communications from an early stage, including clinical, administration and digital staff.
Communication
Ensure robust communication systems are in place for all who are involved in or impacted by the project. Methods of communication used included face-to-face meetings, telephone calls, emails and presentation slides. Communication involved GPs, the local clinical commissioning group, and the Lancashire and South Cumbria Integrated Care System. There was also communication between the services, health informatics and the service provider (UHMB).
Testing
UHMB created a test service on the system to allow the project team to fully test the system prior to go live. This identified some issues with firewalls that needed to be resolved.
Training
LSCFT created an e-learning package based on the one used by UHMB. Time to complete training was a key factor for clinical staff so it is vital that training is relevant and concise.
Ongoing day-to-day support
The project team continued to support the services using the system and assisted with resolving any issues encountered.
Key figures/quotes
Find out more
Key contact
Dr Ayesha Rahim, perinatal psychiatrist, deputy chief medical officer and chief clinical information officer
Disclaimer
These case studies summarise user and patient experiences with digital solutions along the relevant care pathway. Unless expressly stated otherwise, the apps and digital tools referenced are not supplied, distributed or endorsed by NHS England or the Department of Health and Social Care and such parties are not liable for any injury, loss or damage arising from their use.
All playbook case studies have either passed, or are currently undergoing the Digital Technology Assessment Criteria (DTAC) assessment.
Please note the full legal disclaimer: NHS England playbook disclaimer