Supporting GPs with electronic cancer decision support (CDS) tools
Published: 5 July 2021
Cancer decision support (CDS) tools are an aid to clinical decision-making, to assist GPs in their decisions about whether to refer or request further diagnostic investigation in patients where they believe there is a risk of cancer. The tools display the risk of a patient having a specific type of cancer, founded on analysis of a historic population cohort and their risk of having cancer based on a range of factors including symptoms, medical history and demographic data.
Situation
The UK still lags behind other European countries in relation to early diagnosis of cancer, with vague presentation making this more challenging (particularly in relation to cancers which present through vague symptoms). Identifying signs and symptoms at an early stage is therefore essential to reducing mortality and increasing the number of people living beyond a cancer diagnosis.
Aspiration
The aim of the project is to support GPs in their clinical decision making about cancer by making the electronic CDS tool available to all GPs in the UK.
Solution and impact
The CDS tool has been integrated into EMIS Web (utilising Professor Julia Hippisley-Cox’s QCancer algorithm) and is available to all EMIS Web users across the UK. The tool has also been integrated into INPS Vision (using Professor Willie Hamilton’s eRAT algorithm), so is available to all INPS Vision users across the UK.
The CDS tool is a symptom-based software which runs in parallel to a GP’s IT system. It is designed to help GPs to ‘think cancer’ and to aid their clinical decision-making. The tool supports GPs in their decisions about whether to refer or request further diagnostic investigation for patients with a risk of cancer. It displays the risk of a patient having an as-of-yet undiagnosed cancer based on symptomatic information pulled from their patient record. This includes previous symptoms, medical history and demographic data, as well as using live data entered during a consultation.
A prompt arises that is based on the CDS algorithm (either QCancer or eRAT depending on the IT system being used) and then encourages the GP to ‘think cancer’ and follow up with the patient to find out more and consider whether to refer the individual for further tests or investigations.
Impact
The original tool focuses on lung, colorectal, pancreatic, oesophago-gastric, and ovarian cancers. This list has been extended in the EMIS QCancer tool.
These cancers were chosen based on the recommendations of the Macmillan GP adviser team, which felt they were the most appropriate for the electronic tool and would most benefit patients, as they can exhibit vague symptoms.
Following a nationwide pilot in 2013 and further rollout in 2014 to test the feasibility of an electronic CDS tool, the Macmillan GP advisors worked with the 3 main GP IT system providers to develop integrated versions of the tool, with the aim of rolling out the tool to all GPs in the UK.
As of March 2021:
- the integrated QCancer tool is available for EMIS Web users in England and Wales
- the integrated CDS tool is available for INPS Vision users across the UK
- work is taking place with TPP SystmOne to develop an integrated tool
Functionality
The tool has 3 main functions:
- prompts: for each patient with a cancer risk greater than 2%, a prompt appears with the patient’s tumour-specific risk score and the reasoning behind it
- symptom-checker: this is a tumour site-specific template with a list of potential symptoms for the GPs to select. A live risk score is calculated during a consultation incorporating information from the patient record (including previous reported symptoms or test results)
- risk-stratification tool: this tool calculates the risk level for each patient in a practice and allows the practice to review their population in order of risk for each cancer type
Capabilities
- Alert GPs to ‘think cancer’
- Raise awareness of cancer signs and symptoms
- Act as a patient safety net
- Aid continuity of care in practices where a patient may see multiple GPs
- It cannot advise the GP on whether to take action or not
- It cannot replace clinical decision-making
Scope
Can be used in a clinical setting by a healthcare professional.
Key learning points
Integration into the IT systems is key for smooth and efficient running.
All information within the template must be coded and the practice must employ good coding practice to get the best out of the tool.
The positive predictive value (PPV) score, which induces a prompt, must be low enough to encourage GPs to ‘think cancer’ but high enough to ensure that they do not get ‘prompt fatigue’.
Key figures/quotes
The CDS tool received the 2014 HSJ Award for Innovation and Value in Information Technology and the 2015 HSJ Patient Safety Award for Cancer Care, as well as winning the Innovation poster category at the 2015 Royal College of General Practitioners conference in Glasgow.
The CDS tool is built using algorithms from QCancer and eRAT, and both have a weight of evidence behind them. Academic papers supporting this research are available through the Professors who developed the algorithms (Professor Julia Hippisley-Cox for research relating to QCancer and Professor Willie Hamilton for research relating to the eRAT algorithm).
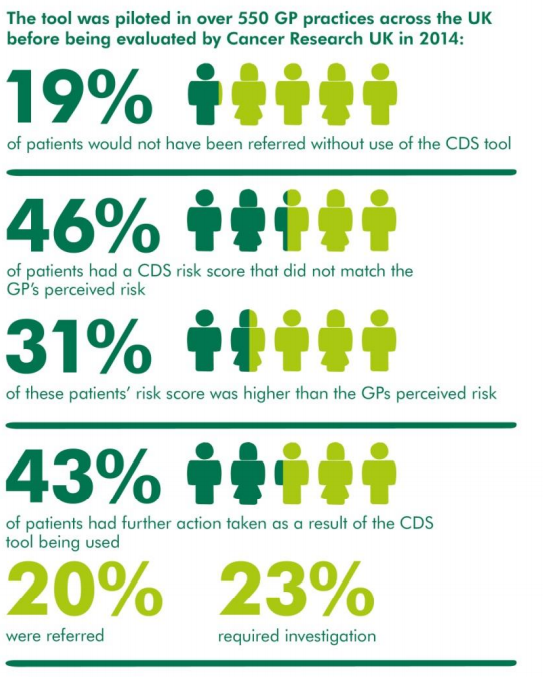
During the 2013 pilot, the aims were to explore the tool’s feasibility in daily practice and its efficacy with regards to patient management. The qualitative and quantitative data from the 2013 pilot evaluation showed some promising evidence around the tool’s efficacy with regards to use in daily practice and patient management:
- GPs reported that around 20% of patients who were referred for further investigation would not have been if the software had not been in place
- GPs indicated that it succeeded in raising awareness of cancer symptoms and alerting them to ‘think cancer’
Find out more
More information on the electronic CDS tool from Macmillan Cancer Support
Read about the CDS tool on the RCGP website
Key contact
Dr Anthony Cunliffe, joint national lead Macmillan GP adviser and joint clinical chair, South East London Cancer Alliance
Sophia Nicola, primary care advisor, Macmillan Cancer Support
Disclaimer
These case studies summarise user and patient experiences with digital solutions along the relevant care pathway. Unless expressly stated otherwise, the apps and digital tools referenced are not supplied, distributed or endorsed by NHS England or the Department of Health and Social Care and such parties are not liable for any injury, loss or damage arising from their use.
All playbook case studies have either passed, or are currently undergoing the Digital Technology Assessment Criteria (DTAC) assessment.
Please note the full legal disclaimer: NHS England playbook disclaimer