Rapid improvement guide to earlier daily discharge times
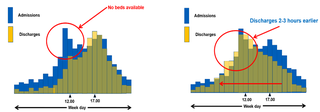
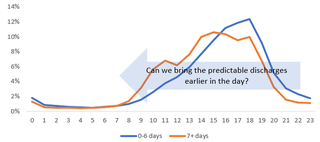
Typically, there’s a mismatch between hospital admissions and discharges. The peak of discharges is often late in the day, preventing early patient flow from emergency departments and assessment units to inpatient wards.
This study highlights the impact discharge timeliness has on hospital crowding and emergency department flow. The conclusion from the study was that enabling more discharges earlier in the day creates capacity for incoming patient flow, reducing time spent waiting for an inpatient bed, reducing hospital length of stay and occupancy. A hospital’s discharge profile needs to more closely mirror its decision-to-admit profile so that beds are available as admission decisions are made. In many cases, changing the discharge profile can have a noticeable impact, so that more patients leave two or three hours earlier each day.
Advice to improve the time of discharge
- Effective use of expected date of discharge (EDD) – The progress of every patient towards their EDD should be assessed and recorded every day at a ward orboard round led by a senior clinical decision maker with multidisciplinary team support. Patients, families and carers should be continually kept up to date, so they know when discharge is expected. Fully informed patients (and their families and carers) will be in a much better position to plan for discharge rather than those that find it a surprise that they are leaving on the day of discharge. To enable beds to be freed up earlier, hospital teams need to prioritise discharge dependent factors whether it be a scan, blood test or something else. Discharge work needs to be urgent, not routine.
- Transport – Ensure transport arrangements are agreed and in place for most patients before the day of discharge. For those patients that need hospital transport, ensure it is booked in advance. Currently, only 10%-20% of requests for hospital transport are before the day of discharge with 80%-90% occurring on the day of discharge (often later in the day) causing significant delays and on occasions an additional overnight stay.
- Take out drugs (TTAs/TTOs) and discharge letters – This is a major constraint to patients waiting on the day of discharge. The majority of TTAs/TTOs should be written up beforehand or finalised during the board/ward round. Involve pharmacy teams to resolve the actual constraints which lead to late TTOs/TTAs and discharge letters within your hospital, the problems will be well known by front line clinical teams.
- Essential equipment – If patients’ EDDs are set effectively and communicated with all members of the multidisciplinary team, it should be a rarity for there to be equipment delays, ordering processes should be standardised and simple.
- Patients requiring support upon discharge – For those patients that require additional care upon discharge, proactive discharge to assess arrangements should be made to prevent discharge later in the day. It is inappropriate for frail older patients to be discharged late in the day, therefore plans should be in place to discharge many of these patients earlier in the day.
- Criteria led discharge – With clear plans (which include physiological and functional criteria for discharge) in medical notes, experienced nurses and AHPs should be able to discharge several patients. Here’s a brief guide to help teams develop criteria led discharge.
- Information to understand and reduce constraints – Use information e.g. the percentage of patients discharged before midday per ward, percentage of TTOs/TTAs on the day of discharge and number of patients utilising hospital transport booked on the day of discharge so clinical and operational teams know how they’re doing and can focus upon specific areas to improve earlier discharge times for their patients. Establish a focus on identifying the root cause of the problem by gaining a true understanding of the constraints in the process. Use data and facts to establish an accurate current state picture, to ensure improvement efforts avoid myths and assumptions.